
CAMH News & Stories
In the headlines or behind the scenes, CAMH stories always aim to inform, engage, and enlighten.
- Home
- CAMH News & Stories

Cool Curling? CAMH VP’s Pursuit of an Olympic Dream
Outside of her roles as VP of Clinical Operations and Chief Nurse Executive, CAMH's Dionne Sinclair has been helping to push the sport of curling in Jamaica beyond the hog line.
About Cool Curling? CAMH VP’s Pursuit of an Olympic Dream$name
About $name
Alcohol causes more harm in Canada than any other drug national expert study finds
Landmark national study is first to assess overall harm of 16 substances
About Alcohol causes more harm in Canada than any other drug national expert study finds
Finding Our People This Blue Monday
In the first few weeks of the year, our initial energetic resolve can wane, and, as winter weeks stretch out before us, symptoms of seasonal blues can set in and present unique challenges that can impact our mental health.
About Finding Our People This Blue Monday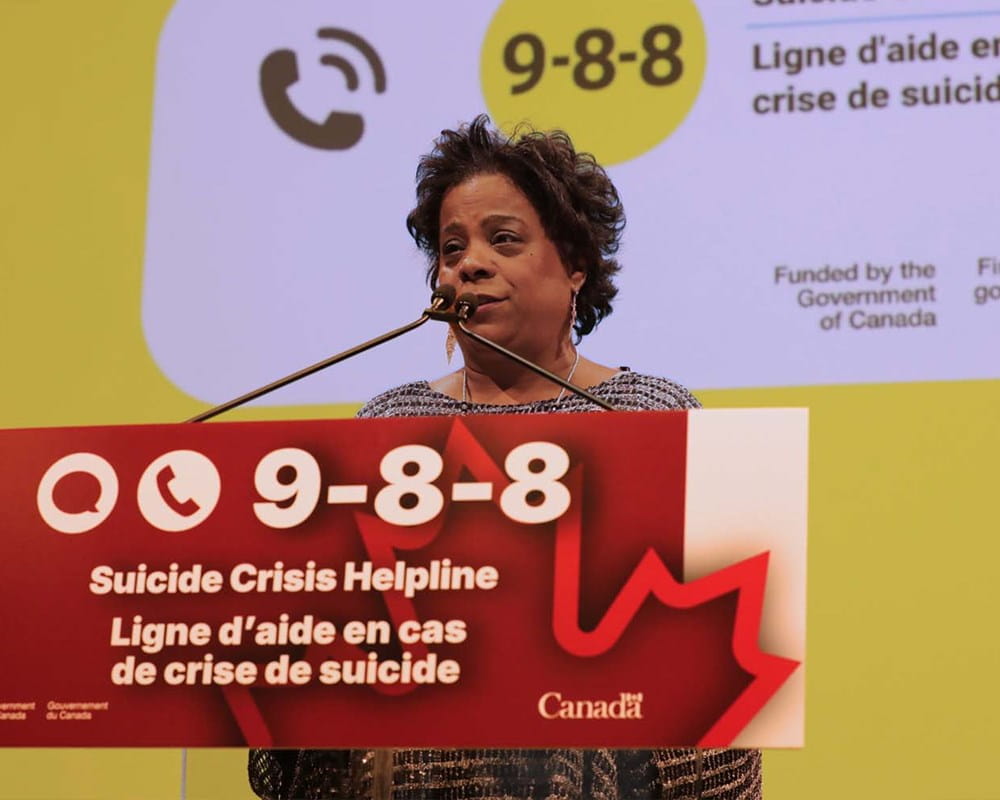
Government of Canada Renews Support for 9-8-8 Suicide Crisis Helpline at CAMH
On Friday January 16th, the Honourable Marjorie Michel, Federal Minister of Health and Parliamentary Secretary Maggie Chi visited CAMH to announce renewed federal support for the 9-8-8: Suicide Crisis Helpline.
About Government of Canada Renews Support for 9-8-8 Suicide Crisis Helpline at CAMH
Five years after the pandemic poor mental health and harmful alcohol use persist in Ontario
CAMH releases data from Canada’s longest-running population-level mental health and substance use surveys
About Five years after the pandemic poor mental health and harmful alcohol use persist in Ontario
Mental Health Apps: What You Need to Know Before You Download
Not All Mental Health Apps Are the Same — And Most Aren’t Backed by Evidence
About Mental Health Apps: What You Need to Know Before You Download
The Next Chapter: Supporting people with substance use disorders as they turn the page from hospital to community
The Next Chapter—a partnership between CAMH and The Neighbourhood Group —provides peer support and intensive treatment for people transitioning from hospital to community after receiving treatment for substance use disorder.
About The Next Chapter: Supporting people with substance use disorders as they turn the page from hospital to community
John Tavares Foundation partners with CAMH Foundation to create brighter futures for youth
CAMH Foundation is thrilled to announce a donation to its lifesaving child and youth work from the John Tavares Foundation, presented in person by NHL Star and Toronto Maple Leafs player, John Tavares and his wife Aryne.
About John Tavares Foundation partners with CAMH Foundation to create brighter futures for youth
CAMH Foundation Appoints Sara Byrnell as Chief Development Officer
CAMH Foundation is pleased to welcome Sara Byrnell as the new Chief Development Officer, effective January 5, 2026. In this newly created role, Sara will lead the national philanthropic strategy, major gift and corporate partnership efforts across the organization.
About CAMH Foundation Appoints Sara Byrnell as Chief Development Officer

